DCLS - Doctorate in Clinical Laboratory Sciences A Force Multiplier for Laboratory Medicine
Brandy Gunsolus1, Brooke M Whitaker1, Kellie A. Vinson1, Leah Ames2, Gurmukh Singh1,2*
1Department of Pathology, Medical College of Georgia, Augusta University, Augusta, USA
2Field Applications Scientist, Thermo Fisher Scientific, USA
*Corresponding author: Professor. Gurmukh Singh, Shepeard Chair in Clinical Pathology and Vice-Chair Pathology, Department of Pathology, Medical College of Georgia, Augusta University, Augusta, GA. 30912, USA; E-mail: gurmukhsinghmdphd@yahoo.com
Received: 24 October 2023; Accepted: 06 November 2023; Published: 10 November 2023
Copyright: © 2023 Gunsolus B. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation:
Abstract
Clinical laboratories depend on phlebotomists, medical laboratory technicians, medical laboratory scientists, information technology specialists, doctoral scientists and pathologists. A new category of healthcare professional, Doctor of Clinical Laboratory Sciences (DCLS), has added another dimension to the operation of the laboratory. The first DCLS professional graduated in 2018 from Rutgers’s University, after her residency training at AU Medical Center. She focused her efforts at improving laboratory utilization which formed the basis of her doctoral degree. Recognizing the significant improvements and cost savings, a second DCLS was recruited in 2020.The contributions of the first two DCLSs have been instrumental in effecting a positive change in (a) cost avoidance of $48 MM from 2018 to 2022, (b) additional revenue of $1.4MM in 2019 (c) introducing a novel patient safety measure of hypercritical values, (d) introduced 91 new tests in-house and achieved cost savings in reference laboratory cost (e) improved diagnostic stewardship by reducing the number of excessive, redundant tests, correcting inappropriate timing of tests and by offering alternative tests with better clinical efficacy (f) served as role models for the medical laboratory science students and improved their recruitment and prompted additional laboratory scientists to pursue enrollment in a DCLS program (g) enhanced experience for pathology residents leading to significant improvement in their examination scores; and most prominently (h) addressed the institutional response to COVID-19 exigency though spearheading testing for the state of Georgia, that has immeasurably elevated the standing of Pathology and Laboratory Medicine among the clinical staff and lay public.
Keywords:
Doctor in Clinical Laboratory Sciences (DCLS); Optimization of Laboratory Use; Cost avoidance; Liaising with clinicians; Hypercritical laboratory values, Long term contract with vendor
Running title: Doctorate in Clinical Laboratory Sciences
- Doctorate in Clinical Laboratory Sciences is a new degree program in laboratory medicine
- The effectiveness of DCLSs in laboratory operations was assessed
- Our experience and survey results were the methods for assessment
- DCLSs are highly effective in improving laboratory utilization and efficiency
- The DLCSs are qualified to respond to exigencies, regulatory changes, and image enhancement
Doctorate in Clinical Laboratory Sciences (DCLS)
Clinical laboratories depend on multiple professionals, e.g., phlebotomists, medical laboratory technicians, medical laboratory scientists (MLS), information technology (IT) specialists, doctoral scientists, and pathologists. A new category of healthcare professional, Doctor of Clinical Laboratory Sciences (DCLS), has added another dimension to the operation of the clinical laboratory. The first DCLS professional graduated in 2018 from Rutgers’s University, after having completed her residency training at a university affiliated medical center in Southeastern USA. She focused her efforts at improving laboratory utilization which formed the basis of her doctoral degree and added additional quality improvement measures at this institution. Recognizing the significant improvements and cost savings that this new role provided a second DCLS was recruited in 2020.
The primary mission of clinical laboratories is to promptly provide accurate results from testing patient materials to the primary clients, the bedside healthcare providers. The additional mission of laboratory stewardship, now a regulatory requirement of the Office of Inspector General, includes improving efficiency, cost effectiveness, and adding to the medical knowledge of laboratory medicine. These missions are carried out by a multidisciplinary team. A new category of professional, the DCLS, has entered the enterprise. The first DCLS degree recipient in the USA graduated from Rutgers University in May 2018 and continued on as the Laboratory Utilization Manager at this institution. The second DCLS resident joined the medical center in June 2019 and graduated in May 2020 and continued here as Manager of Microbiology and Pathology Laboratory Utilization [1].
DCLS programs
The advanced practice doctorate in clinical laboratory sciences trains certified medical laboratory scientists to become contributing members of the front-line interdisciplinary healthcare team, perform outcomes-based research in clinical diagnostics, and provide evidence-based recommendations for appropriate utilization of clinical laboratory testing. Three universities currently offer such programs: Rutgers, New Jersey, University of Texas Medical Branch - Galveston, Texas, and University of Kansas, Kansas [1].
The DCLS curriculum includes graduate level courses, consisting of 70-80 credit hours, in clinical laboratory sciences, such as, chemistry, hemostasis, pharmacology, pathophysiology, research (i.e., data analysis, principles of translational and outcomes research), professional development, clinical laboratory utilization, and healthcare regulations. The didactic part of the education may be completed mostly on-line or on-site through a continuous presence or multiple short episodes. A one-year full-time, on-site clinical practice/residency is required and includes a research project aimed at quality improvement. The training culminates with the candidate defending the thesis resulting from the year of on-site residency [2].
Residency training
The final year of the DCLS program is a one-year, full-time clinical practice/residency that focuses on four areas: Patient Care Teams (PCT), Diagnostic Management Teams (DMT), Utilization Review (UR), and Community Intervention (CI). For PCT, the DCLS resident participates in patient care rounds to provide information on all phases of testing, including but not limited to, appropriate specimen choice, timing of testing, medical necessity of testing, and test interpretation. DMT is the convening of an interdisciplinary team to formulate patient-centered algorithmic testing, and for diagnosis and management of hard to diagnose and treat conditions, efficiently. In an enhanced mode, this has resulted in face-to-face diagnostic management teams, much like anatomic tumor boards but for clinical pathology issues, pioneered at a training program in Galveston TX. UR encompasses the review of laboratory generated reports looking for appropriateness of orders, mis-utilization of testing, overutilization of testing and underutilization of testing. Additionally, the DCLS resident participates alongside clinical pathology residents to review send-out tests for medical necessity when the cost per test is > $150 [3]. CI occurs through the Lab Tests Online website, where the DCLS answers laboratory related questions in the discipline of choice from the public at large [4]. Tandem to these four areas, the DCLS resident also conducts a research project specific to the clinical laboratory and laboratory medicine that is presented at the end of the program.
The Medical Center
The collaborative partnership with the Rutgers University DCLS program took place at a medical school affiliated hospital with 478 adult beds, 150 pediatric beds and approximately 90 outreach clinics. The medical center is a tertiary care hospital with open heart surgery, neurosurgery, solid organ and bone marrow transplant, dialysis, and other tertiary care services. The medical center is the Level 1 trauma center for the region, and also serves the prison population for the state.
DCLS deployment
The first DCLS, having completed her residency at the medical center got a running start in her role as the Laboratory Utilization Manager for the medical center clinical laboratory. The second DCLS resident worked alongside the Laboratory Utilization Manager assisting her in her ventures and completed a quality improvement project by addressing hypercritical laboratory values leading to the activation of rapid response teams initiated by laboratory personnel.
Each of the ventures in which a DCLSs played a leading or major or contributory role, at this medical center, are addressed below:
Accuracy and Timeliness
As is the usual practice and mandated by regulation, the laboratory maintains a quality management program to ensure accuracy and timeliness of results. The DCLSs are part of the Quality Management Team. Timeliness of reporting results was enhanced through a judicious combination of automation and selected deployment of point-of-care testing. As reported earlier, all routine tests that could reasonably be ordered STAT have an in-laboratory turn-around time of <45 minutes for more than 90% of the specimens [5]. This performance has allowed us to eliminate “stat” tests. Improvement in accuracy of the testing is evidenced by the paucity of failure in proficiency testing, and lack of Phase II deficiencies pertinent to the accuracy of testing in the last accreditation inspection by the College of American Pathologist (CAP). The DCLS professionals have been instrumental in implementing enhanced standards in accuracy, for example, in proficiency testing if the results exceed by Standard Deviation Index of one (1SDI) on one side of the mean in 4 of 5 specimens, the supervisors are required to investigate and implement corrective actions to address the apparent bias.
Interdisciplinary team testing and treatment algorithm development has further decreased overall turnaround time to reduce time to diagnosis and improve time to treatment. Interdisciplinary testing and treatment algorithms implemented by the DCLSs include adult and congenital syphilis algorithms, Clostridium difficile algorithm, alpha-1-antitrypsin algorithm, and heparin induced thrombocytopenia algorithm.
Laboratory Utilization
Optimization of laboratory utilization was the topic of the first DCLS’s thesis during her residency. While the concept is not novel, the execution of this venture often falters due to resistance from multiple parties. The DCLS established rapport with health care professionals in family medicine, internal medicine, critical care, cardiology, infectious disease, pulmonology, and pediatrics programs during her residency through rounding with the residents and attendings in these specialties. The approach involved discouraging the overuse of panels, avoiding unnecessary repeat testing, promoting use of appropriate tests, and providing consultation in test selection and interpretation [6]. (A poster on this topic received the first-place award at the 2020 annual ASCLS/AGT Joint Annual Meeting.) Examples of such activities are described below:
1. Panels of tests: In consultation with the Chief Medical Officer (CMO) and the approval of the Medical Executive Board (MEB), a number of changes were implemented in the use of panels of tests. Testing for comprehensive metabolic profile (CMP), complete blood cell count (CBC) with differential and basic metabolic panel (BMP) was limited to once a day, with exceptions for the first 24-hours after admission, and critical care units. Panel testing for thrombophilia was discontinued for in-patients. The laboratory had an existing algorithm for white blood cell differential testing and is in the process of implementing next generation Hematology, in collaboration with Beckman-Coulter, for further reducing the number of manual differential white blood cell counting episodes. Orders for daily testing for x number of days, e.g., BMP, CMP, CBC with differential etc. were inactivated, except in critical care areas [7].
2. Limitation on repeat testing: Testing for A1c was limited to once in 45 days and if a test was ordered sooner, results of the most recent test were displayed with a request to withhold the order. A1c test post-red cell transfusion was also eliminated. Repeat testing for genetic tests, including Factor V Leiden, Prothrombin gene mutation, was terminated, and each repeat order displayed the results of earlier testing [8,9].
3. Algorithmic testing: An algorithm was developed and implemented for tests for auto-immune disorders and orders for a wide-ranging panel were discontinued. (Figure 1) This was in addition to the algorithmic testing for serum protein electrophoresis, immunofixation and serum free light chain tests already in use [10-18].

Figure 1: Algorithmic approach to ANA testing for appropriate utilization of the tests.
4. Optimization of microbiology testing: The laboratory implemented molecular testing for a panel of respiratory pathogens, and the DCLS, in collaboration with pediatrics limited testing to influenza and respiratory syncytial virus testing only when testing for the full 21 pathogen respiratory panel was not warranted. The DCLS led the investigation for use of procalcitonin testing in the diagnosis and management of sepsis, in collaboration with pharmacy. The team collected enough cogent information to effect discontinuation of the test, except for pediatric patients. By converting to molecular testing rather than conventional cultures, surveillance cultures for MRSA were eliminated. Molecular testing for about 20 pathogens, each, in respiratory and gastro-intestinal has reduced costs, and shortened the turn-around time for diagnoses. Rapid diagnosis and ruling out of communicable infections have reduced hospital costs by limiting the use of isolation rooms.
5. Vitamin K utilization: Daily laboratory utilization review by the 2019-2020 DCLS candidate revealed a quality gap around appropriate testing for vitamin K status in Bariatric Surgery patients that was both expensive and time-consuming. The DCLS resident provided the Bariatric Surgery Service with an evidence-based recommendation and interpretation of the American Society for Metabolic and Bariatric Surgery guideline to ensure patients are receiving quality care utilizing the most appropriate test for vitamin K status both pre- and post-op was PT/PTT and INR. Reference lab orders for vitamin K in Bariatric Surgery patients declined from 30 in July 2019, to one in August 2019 and zero thereafter. Additionally, turn-around-time and facility costs were reduced by performing the in-house PT/INR. Turn-around-time was reduced from three days (reference laboratory) to less than one hour (in-house).
6. Syphilis algorithm: Questions arose from labor and delivery around how to interpret maternal syphilis results and when newborn treatment of syphilis was recommended. Working with pediatric infectious disease healthcare professionals, the DCLSs developed an algorithm to include both maternal testing and newborn treatment. The algorithm helped ensure that newborns were not being discharged prematurely without treatment.
7. Esoteric/reference laboratory testing: Special emphasis was placed on promoting appropriate utilization of esoteric tests that needed to be sent to a reference laboratory. The DCLSs, in working with the various specialists in general, and neurologists, pediatricians and rheumatologists, in particular, developed a list of esoteric tests that would have automatic approval, if ordered by the appropriate specialist. All other tests that needed to be sent out and had a cost per test exceeding $150.00/test were reviewed by the clinical pathology residents under the guidance of the DCLS and clinical pathologists. The integration of the residents in review of esoteric testing was implemented primarily by the DCLS in collaboration with the pathology residency training director. The number of consults referred to pathology residents was limited to no more than three per day to ensure that residents had enough time to research the issues [3]. The effective limitation of unnecessary testing resulted in a cost avoidance of $311,009 by pathology residents and $857,142 by the DCLSs for a total of $1.17 M during 2018-2022.
Through continual review of esoteric test utilization, the DCLSs led the process for insourcing of 91 tests during 2019-2022, e.g., alpha 1 anti-trypsin, Quantiferon Gold TB testing, Fecal Immunochemical test for human globin (FIT) for colon cancer screening, IgG subclasses, ceruloplasmin, Mumps IgG, calprotectin, pancreatic elastase, IGF-1, HPV PCR, HSV 1 & 2 PCR, renin and aldosterone and 72 tests related to allergy and immunology testing.
8. Revenue enhancement: In collaboration with laboratory section managers and hospital billing service, the DCLSs systematically reviewed the amounts billed, denials and collections for laboratory services. Each month they analyzed the top three offenders that impaired revenue collection and instituted corrective measures. Examples of the measures included correction of CPT codes, ensuring correct usage of HCPCS codes, and educating physicians regarding ICD-10 diagnosis codes for laboratory testing. This process is an ongoing venture; however, in 2019 alone the revenue was enhanced by $1.4 MM. A 40.5% reduction in laboratory service payment denials was realized by 2022.
9. Recruitment of MLS: The DCLSs have developed close collaboration with the Department of Medical Laboratory Sciences and promoted the rotation of MLS students through the clinical laboratory of the hospital. The exposure to the excellent work environment and potential for career development has resulted in many of the MLS students staying with the laboratory. Through their exposure in usual and social media, additional DCLS students have elected to get their residency training at the hospital.
10. Laboratory automation: In parallel with the recruitment of DCLSs, the laboratory entered into a long-term contract with Beckman-Coulter and its parent company, Danaher, that included automation in the Core laboratory covering Chemistry and Hematology. The efficiencies introduced by automation allowed us to provide the service with about 25% fewer personnel. The combination of savings in personnel costs, reference laboratory cost reduction, optimization of laboratory test use and revenue enhancements resulted in a net gain to the hospital of about $48MM over four years.
Hypercritical laboratory values and laboratory-initiated activation of rapid response teams
The 2019-2020 DCLS resident identified this topic as the subject of her thesis [19]. In collaboration with the Chief Medical Office, Emergency Department, and Nursing Service the DCLS resident, with the support of laboratory leadership, identified the laboratory parameters to be designated as hypercritical values, that should be immediately communicated to the appropriate medical provider(s) (Figure 2).
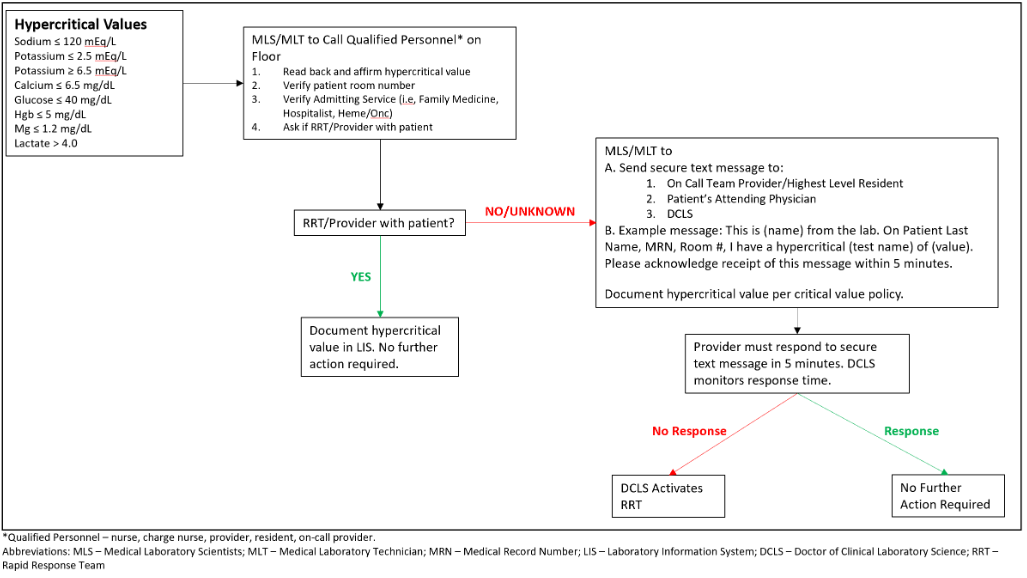
Figure 2: Rapid response team activation for hypercritical values.
In this hypercritical value notification protocol, the laboratory MLS/MLT reporting the hypercritical value to qualified personnel (i.e., nurse, nurse manager, provider), inquired if the patient’s provider and/or rapid response team (RRT) was already in the patient’s room and verified the patient’s room number and admitting service (e, g., Family Medicine, Hospitalist, Internal Medicine). If the provider and/or RRT were already with the patient at the time of the hypercritical value notification, the MLS documented notification per the current critical value notification policy and no additional action was required. If the provider and/or RRT was not with the patient at the time of hypercritical value notification, or if this information was unknown, the MLS/MLT sent a secure text message to the patient’s on-call provider, attending physician, and DCLS. At this point the provider(s) had five minutes, monitored by the DCLS, to acknowledge receipt of the message by responding to the secure text message which went to the DCLS. If the provider(s) responded within five minutes, no further action was taken. If the provider(s) did not respond within five minutes, the DCLS activated the RRT.
The use of this escalated provider notification with RRT activation by the DCLS was studied as a quality improvement and patient safety initiative. Data for three months, each, prior to and after the intervention were analyzed. Evaluation of this process was to determine if improving time to intervention for hypercritical values could decrease length of stay, ICU admission, and in-patient mortality. ANCOVA analysis of time to treatment ordered from provider aware F = 0.155, ρ = 0.696, partial eta squared = 0.004 showed no significant difference in time to treatment ordered between the two groups. Time to treatment given from provider aware F = 0.707, ρ = .406 and partial eta squared = 0.021 also showed no significant difference between the pre- and post-implementation groups. Length of stay, F = 0.183, ρ = 0.620, and partial eta squared = 0.002 showed no significant difference between the two groups. Additional analysis was done from time hypercritical called to time treatment ordered and time treatment is given. Time to treatment order was significantly different for the two groups, F = 5.864, ρ = 0.018, and partial eta squared = 0.086. The adjusted mean time to treatment order was approximately 90 minutes quicker in the post-intervention population. Analysis of ICU admissions and RRT activation could not be performed due to a lack of sufficient data. On average the post-intervention group spent two fewer days in the hospital.
Overall, the null hypothesis stands due to the lack of statistical significance demonstrated. However, it was evident that there was a trend toward improving time to intervention and decreased length of stay from the results of this study. The impact on ICU admission and in-patient mortality could not be demonstrated in the small cohort studied. The data from this study supports further investigation of escalated provider notification of hypercritical values using secure text messaging and RRT activation by the DCLS/Laboratory.
Pathology Residency Training Enhancement
In addition to the aforementioned review of esoteric testing and educating the residents about the process, the DCLS, in collaboration with the Pathology Residency Program Director has implemented an on-going quality management review of practices. The quality management and process improvement projects carried out by the residents have included, effect of blood transfusion on laboratory testing, selection of optimal equipment for intra-operative heparin monitoring, implementation of point-of-care testing for substances of abuse in psychiatry, scholarly review of serum folic acid testing, laboratory explanation for obesity paradox, accuracy of monoclonal immunoglobulin measurement, optimization of reporting of critical values, and modification of protein electrophoresis procedure to enhance sensitivity of detection of monoclonal light chains in serum and urine, etc. In addition to improving utilization these enhancements resulted in improved performance by pathology residents in their in-service examination scores (RISE). RISE scores in Chemistry and Laboratory Administration increased by 40% and 50% respectively. There were 12 publications in clinical chemistry since the implementation of the new curriculum, while there were no publications in clinical chemistry, by the program residents in the 5-year period prior to the new curriculum [20-31].
Liaising with clinical colleagues
Starting with her residency training, the first DCLS has regularly rounded with various clinical specialties and established her bona fide as an expert in appropriate laboratory utilization. For all of these healthcare professionals, this was their first introduction and exposure to working with a DCLS. Research in this area demonstrated that provider perceptions of the DCLS evolved from having no understanding of this new healthcare professional to recognizing her as a bona fide expert in appropriate laboratory utilization [6]. The DCLS role has been instrumental in providing recommendations for appropriate testing rather than just curtailing testing. She has been invited by the medical specialties of neurology, infectious disease, pulmonology, cardiology, emergency medicine, family medicine, internal medicine, rheumatology, and pediatrics to deliver formal talks on appropriate laboratory testing. Through her dedication and inspired value-added service she has come to be recognized as a resource for enhancing patient care and safety.
Covid-19 Exigency
The extraordinary circumstance of the SARS CoV-2 pandemic provided a unique opportunity for the DCLSs and the laboratory to showcase the importance of accurate and timely diagnosis. The DCLSs, in collaboration with the Clinical Microbiology Laboratory Director, took the lead in procuring equipment and supplies for testing for the virus and antibodies to the virus. It was their tireless effort that allowed the Medical Center to provide this service to whole state of Georgia and allowed the governor to be the first state in the US to start opening businesses with appropriate quality controls and safety protocols [32,33]. Their role was lauded by the university leadership and brought unprecedented recognition to the importance of diagnostic laboratory. This recognition extended to the National Golf tournament and the medical center provided COVID-19 testing for the golf tournaments.
Voice of the DCLS
A survey of DCLS professionals who have been employed for at least one year following their graduation was conducted. There were about 15 eligible participants and seven of them completed the survey questionnaire. Questions revolved around participants’ experiences that a DCLS degree provided an additional career advancement opportunity that would not have been attainable as a medical laboratory scientist. Additional questions addressed participants perceived value and contributions to patient care amongst their healthcare colleagues. Their perceptions and opinions are summarized below:
Q: Participants were asked to list their job titles, before and after working as a DCLS
| Previous Job Titles (pre-DCLS degree) | New Job Titles (post-DCLS degree)* |
|---|---|
| Laboratory Director (moderate complexity) | VP of US Clinical Operations |
| Hematology and Flow Cytometry Supervisor | Scientific Engagement and Clinical Education Associate |
| Administrative Officer | Adjunct Faculty |
| Department Administrator | Associate Laboratory Director |
| Laboratory Manager | Program Manager |
| Chief Medical Technologist | Chief Medical Technologist |
| Administrative Laboratory Director | Laboratory Director and Technical Consultant |
| *post-DCLS job titles are not necessarily listed to match with the corresponding pre-DCLS job title. | |
Additional questions were presented with responses requested using a Likert scale. Participants were asked to rank their responses on a scale of 0 to 9 with 9 being “very strongly” The results of the survey are presented in Table 1. There were no responses at Likert level of 6 or lower attesting to the satisfaction with their experience, recognition of their worth and their perception of being productive members of the healthcare teams.
Table 1: Summary of survey question results. The response of the DCLSs was overwhelmingly positive about their training experience and improvement in work conditions following graduation.
|
|
Responses on Likert scale of 0-9, % |
|||
|
Survey Questions |
9 |
8 |
7 |
6 and lower |
|
Satisfaction with the quality of training received from your DCLS program |
72 |
14 |
14 |
0 |
|
Improvement in your quality of life after graduation from the DCLS program |
71 |
29 |
0 |
0 |
|
Improvement in professional satisfaction in your career |
72 |
14 |
14 |
0 |
|
Improvement in your perception of self-worth in the healthcare field |
43 |
29 |
29 |
0 |
|
The positive change in your perception of how you are recognized/appreciated for your contribution to healthcare |
57 |
14 |
29 |
0 |
|
When working with PhD-level laboratory professionals, how positive have your interactions been impacted with your contributions as a DCLS? |
57 |
14 |
29 |
0 |
|
When working with Pathologists, how positive have your interactions been impacted with your contributions as a DCLS? |
43 |
43 |
14 |
0 |
|
When working with non-laboratory Physicians, how positive have your interactions been impacted with your contributions as a DCLS? |
86 |
14 |
0 |
0 |
|
How strongly do you feel that becoming a DCLS has improved your ability to create positive changes in laboratory medicine? |
72 |
14 |
14 |
0 |
|
How strongly do you feel that becoming a DCLS has opened career opportunities that were not an option as a Medical Laboratory Scientist? |
57 |
43 |
0 |
0 |
Participants were also asked the following questions and were provided the opportunity to provide free-text responses:
Q: Since graduating from your DCLS program, what is the single-most impactful item that you have accomplished?
| Created a test utilization model for Vit D, Thyroid panel, and coagulation testing. |
| Poster presentations at the 2022 AACC |
| Adjunct faculty and revamped immunology and microbiology courses |
| New position requiring a doctorate |
| Liaison between labs and clinical providers |
| Instituted many new ordering practices using evidence-based practice |
| I am laboratory director, and I actually get the credit for the hard work I do… |
Q: How would you respond to this statement:
"The DCLS program is important for improving career opportunities for medical laboratory scientists."
| I do not think the DCLS is a natural progression for all MLSs. But for those that want to breach the lab silo, use their knowledge, improve healthcare in all aspects of the patient cycle, and collaborate with all areas of medicine…there is now a place a for you. |
| True |
| It is important to provide a career ladder, but it isn't for everyone. We need to make sure this isn't a degree field people pursue if they aren't willing to fight for the lab. |
| Agree, very important |
| Agree |
| The DCLS is one route for people who want to practice clinical laboratory science at an advanced level. However, it will not strongly widen the field as there is already a shortage of scientists. Having additional opportunities is very important for some people and we in the laboratory should have a seat at the table, especially when/if the pathologist you work with is very AP focused. |
Q: Do you have any comments regarding your DCLS experiences that you would like to add?
| The DCLS is not meant to replace a pathologist or PhD. It is a needed supplement that has a place in medicine and the laboratory. |
| I love the laboratory. It has been my career, and I am very passionate about my education, my knowledge about the profession and the patients that I affect every day. This degree changed my career path, and I wouldn't change the path that I chose. It is so important that we get the medical community to see the worth of not only the DCLS, but medical laboratory scientists as a whole, so that the work we do and the quality we bring to the field does not go unnoticed. |
Conclusion
We recognize that many of the measures addressed and implemented by the DCLS are not novel or unique; however, as professionals with responsibility for promoting appropriate laboratory utilization, liaising with bed-side clinicians and trainees, creating a laboratory-initiated rapid response protocol for hypercritical values, and leading the response to the COVID-19 pandemic, the DCLSs brought about a paradigm shift in the way the clinical laboratory is viewed by its primary clients, the healthcare providers. It is through the efforts and influence of the DCLSs that the clinical laboratory is consulted by providers seeking to improve laboratory testing for their patients. The latest example of such a collaboration has been to introduce point of care testing for a new clinic that manages substance abuse disorders. In the military parlance, the DCLSs have been force multipliers in leveraging the efforts of the clinical laboratory in reducing turnaround time, optimizing the reporting of critical values, promoting appropriate lab test utilization, and most importantly, spotlighting the significant contribution of laboratory medicine among our clinical colleagues and the lay public [34,35].
The DCLSs have been instrumental in promoting the appreciation for clinical laboratories by healthcare providers and the lay public through their performance and expert use of media to highlight the critical role of laboratory in healthcare. They are valued by the hospital for their results in reducing costs and improving the efficiency of clinical laboratories. The hospital and the associated medical school have both benefitted from this collaboration with Rutgers and the mutually beneficial relation continues while promoting patient safety, improving diagnostics, and providing a vital contribution to public health.
Disclosure
Professor. Gurmukh Singh, serves as a consultant to Beckman-Coulter, Sebia, Diazyme and HealthTap.
References
1. Singh G. Optimization of Laboratory Utilization: A Unique Role for the Doctor of Clinical Laboratory Science. Clinical Lab Manager. Today’s Clin Lab. April 27, 2020. https://www.clinicallab.com/optimizing-lab-talent-a-unique-role-for-the-doctor-of-clinical-laboratory-science-22504
2. Doctor of Clinical Laboratory Science. Rutgers school of Health Professionals. https://shp.rutgers.edu/clinical-lab-and-imaging-sciences/doctorate-of-clinical-lab-science/
3. Greenblatt MB, Nowak JA, Quade CC, Tanasijevic M, Lindeman N, et al. Impact of a prospective review program for reference laboratory testing requests. Am J Clin Pathol. 2015 May;143(5):627-34. https://doi.org/10.1309/AJCPN1VCZDVD9ZVX
4. Lab Tests Online. Association for Diagnostics & Laboratory Medicine. https://www.aacc.org/advocacy-and-outreach/lab-tests-online
5. Singh G, Savage NM, Gunsolus B, Foss KA. Requiem for the STAT Test: Automation and Point of Care Testing. Lab Med. 2020 Mar 10;51(2):e27-e31. https://doi.org/10.1093/labmed/lmz080
6. Ames L. Perceptions of Collaboration With a Doctor of Clinical Laboratory Science (Doctoral dissertation, Northern Illinois University). 2020; 27963361. https://huskiecommons.lib.niu.edu/allgraduate-thesesdissertations/6812
7. Salinas M, López-Garrigós M, Flores E, Leiva-Salinas C. Serum Uric Acid Laboratory Test Request Patterns in Primary Care: How Panels May Contribute to Overutilization and Treatment of Asymptomatic Patients. Lab Med. 2018 Jan 1;49 (1):55-8. https://doi.org/10.1093/labmed/lmx075
8. Patel T, Karle E, Krvavac A. Avoiding unnecessary repeat laboratory tsting. Cureus 2019 Oct 9;11(10); 11e5872. https://doi.org/10.7759/cureus.5872
9. Pivovarov R, Albers DJ, Hripcsak G, Sepulveda JL, Elhadad N. Temporal Trends of Hemoglobin A1c Testing. J Am Med Inform Assoc. 2014 Nov 1;21(6):1038-44. https://doi.org/10.1136/amiajnl-2013-002592
10. Heaton C, Vyas SG, Singh G. Audit of use and overuse of serum protein immunofixation electrophoresis and serum free light chain assay in tertiary health care: a case for algorithmic testing to optimize laboratory utilization. Amer J Clin Pathol. 2016 Apr 1;145(4):531-7. https://doi.org/10.1093/ajcp/aqw026
11. Kavanaugh A, Tomar R, Reveille J, Solomon DH, Homburger HA. Guidelines for clinical use of the antinuclear antibody test and tests for specific autoantibodies to nuclear antigens. Arch Pathol Lab Med. 2000 Jan 1;124(1):71-81. https://doi.org/10.5858/2000-124-0071-GFCUOT
12. Tozzoli R, Bizzaro N, Tonutti E, Villalta D, Bassetti D,et al. Guidelines for the laboratory use of autoantibody tests in the diagnosis and monitoring of autoimmune rheumatic diseases. Am J Clin Pathol. 2002 Feb 1;117(2):316-24. https://doi.org/10.1309/Y5VF-C3DM-L8XV-U053
13. Satoh M, Vázquez-Del Mercado M, Chan EK. Clinical interpretation of antinuclear antibody tests in systemic rheumatic diseases. Mod Rheumatol. 2009 Jun 1;19(3):219-28. https://doi.org/10.3109/s10165-009-0155-3
14. Stinton LM, Fritzler MJ. A clinical approach to autoantibody testing in systemic autoimmune rheumatic disorders. Autoimmun Rev. 2007 Nov 1;7(1):77-84. https://doi.org/10.1016/j.autrev.2007.08.003
15. Hoffman IE, Peene I, Meheus L, Huizinga TW, Cebecauer L, et al. Specific antinuclear antibodies are associated with clinical features in systemic lupus erythematosus. Ann Rheum Dis. 2004 Sep 1;63(9):1155-8. https://doi.org/10.1136/ard.2003.013417
16. Colglazier CL, Sutej PG. Laboratory testing in the rheumatic diseases: a practical review. South Med J. 2005 Feb 1;98(2):185-91. https://doi.org/10.1097/01.SMJ.0000153572.22346.E9
17. Van Den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, et al. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum. 2013 Nov;65(11):2737-47. https://doi.org/10.1002/art.38098
18. Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, et al. International Sjögren's Syndrome Criteria Working Group. 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjögren's syndrome: A consensus and data-driven methodology involving three international patient cohorts. Ann Rheum Dis 2017 Jan;69(1):35-45. https://doi.org/10.1002/art.39859
19. Newitt VN. Labs add safety net to critical values procedure. CAP Today. March 2019. https://www.captodayonline.com/labs-add-safety-net-to-critical-values-procedure/
20. Haldiman L, Zia H, Singh G. Improving Appropriateness of Blood Utilization Through Prospective Review of Requests for Blood Products: The Role of Pathology Residents as Consultants. Lab Medicine. 2014 Aug 1;45(3):264-71. https://doi.org/10.1309/LMSKRN7ND12ZOORW
21. Larsen R, Allen S, Thompson TZ, Bollag R, Singh G. Challenges in Interpreting Multiple Monoclonal Bands on Serum Protein Electrophoresis and Serum Immunofixation Electrophoresis: an Illustrative Case Report. J Appl Lab Med. 2019 Nov 1;4(3):455-9. https://doi.org/10.1373/jalm.2018.027938
22. Lee W, Singh G. Serum free light chain assay in monoclonal gammopathies. Lab Med. 2019;50:381-389. https://doi.org/10.1093/labmed/lmz007
23. Thompson TZ, Kunak RL, Savage NM, Agarwal S, Chazelle J, Singh G. Intra-operative monitoring of heparin: Intraoperative Monitoring of Heparin: Comparison of Activated Coagulation Time and Whole-Blood Heparin Measurements by Different Point-of-Care Devices with Heparin Concentration by Laboratory-Performed Plasma Anti-Xa Assay. Lab Med. 2019 Oct 10;50(4):348-56. https://doi.org/10.1093/labmed/lmz014
24. Clavijo A, Ryan N, Xu H, Singh G. Measurement of monoclonal immunoglobulin protein concentration in serum protein electrophoresis: Comparison of automated versus manual/human readings. Lab Med. 2020 May 6;51(3):252-8. https://doi.org/10.1093/labmed/lmz055
25. Kozman D, Mattox S, Singh G. Serum folate of less than 7.0 ng/mL is a marker of malnutrition. Lab Med. 2020 Sep 1;51(5):507-11. https://doi.org/10.1093/labmed/lmz101
26. Nwogbo OV, Ullah A, Singh G. Obesity Paradox: Laboratory findings in uncomplicated obesity. Is bias a plausible explanation? J Appl Lab Med. 2021 Jan;6(1):113-8. https://doi.org/10.1093/jalm/jfaa049
27. Ullah A, Omar N, Savage NM, Bollag RJ, Singh G. Immune subtraction for improved resolution in serum protein immunofixation electrophoresis and antibody isotype determination in a patient with autoantibody. Pract Lab Med. 2021 Aug 1;26:e00240. https://doi.org/10.1016/j.plabm.2021.e00240
28. Jin Y, Savage NM, Bollag RJ, Xu H, Singh G. Light chain multiple myeloma: High serum free light chain levels portend renal damage and poorer survival. J Appl Lab Med. 2021 Nov 1;6(6):1592-600. https://doi.org/10.1093/jalm/jfab090
29. Wilhite D, Arfa A, Cotter T, Savage NM, Bollag RJ, et al. Multiple Myeloma: Detection of free monoclonal light chains by modified immunofixation electrophoresis with antisera against free light chain. Pract Lab Med. 2021 Nov 1;27:e00256. https://doi.org/10.1016/j.plabm.2021.e00256
30. Singh G, Whitaker BM, Wu AH, Xu H, Bollag RJ. Serum free light chain quantification testing: Comparison of Binding Site and Diazyme methods for disease monitoring. J Appl Lab Med. 2022 Nov 1;7(6):1290-301. https://doi.org/10.1093/jalm/jfac068
31. Singh G, Arinze N, Manthei DM, Plapp FV, Bollag RJ. Urine protein immunofixation electrophoresis: Free light chain urine immunofixation electrophoresis is more sensitive than conventional assays for detecting monoclonal light chains and could serve as a marker of minimal residual disease. Lab Med. 2023 Sep 1;54(5):527-33. https://doi.org/10.1093/labmed/lmac155
34. Singh G, Bollag R, Kolhe R, McMullen A, Savage NM. Engaging pathology residents in scholarly activities. J Appl Lab Med. 2021 Mar 1;6(2):567-9. https://doi.org/10.1093/jalm/jfaa094
35. Singh G, Bollag RJ, Savage NM. Engaging Pathology Residents in Clinical Chemistry: The Essential Ingredient Is a Committed Teacher. J Appl Lab Med. 2021 Mar 1;6(2):522-31. https://doi.org/10.1093/jalm/jfaa140
